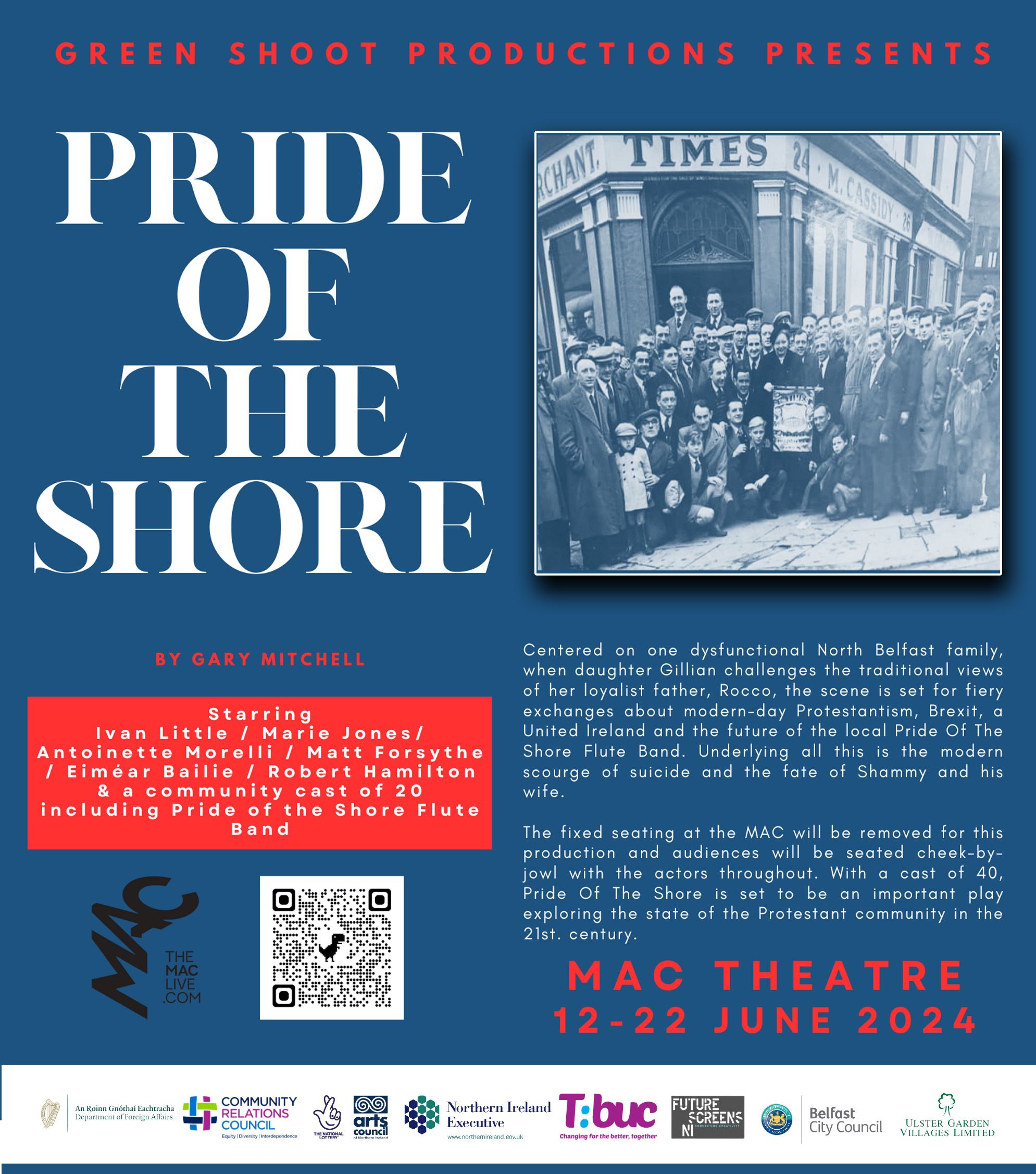
THE latest corruptions of democracy swirling around Westminster should not distract us from the intensifying crises in public services, especially health, none of which look like going away soon. The state of the NHS is so bad that radical alternatives to the free-at-the-point-of-use model are openly debated. The voices of private provision get louder and “solutions” such as rationing through fees are getting serious air time. Former chancellor (for six months), Sajid Javid, has even suggested that Britain should be more like Ireland (26 counties) and introduce charges for seeing a GP and for attending A&E without a GP referral. The trouble with the NHS, he wrote in The Times, was that “the only rationing mechanism is to make people wait”. Apply the market mechanism of charges and – bingo! – the queues at emergency departments and for GP appointments magically disappear. Shows how much he knows about Ireland.

SAJID JAVID
— Carol Vorderman (@carolvorders) January 21, 2023
Aug 20 Starts as paid adviser to investment bank JP MORGAN
May 21 JPM forms Morgan Health
June 21 Javid is Health Secretary
Nov 22 Morgan Health says aggressively investing in “promising healthcare companies”
Jan 23 Javid calls for NHS reform!https://t.co/oNt9T3BTKv
There is another choice of direction for the NHS which is to invest more in public health. This includes health promotion and disease prevention. Promoting good health means, for example, encouraging exercise through sports facilities, parks and clubs at all stages in the life cycle, as well as good education about sex, drugs (including alcohol) and diet. And yes, prime minister, it means wearing a seat belt.
Oh look, here’s the PM happily broadcasting himself breaking the law.
— Supertanskiii (@supertanskiii) January 19, 2023
"The law states that you must use a seat belt if fitted unless you qualify for a medical exemption"
This even applies if using a booster seat, like Sunak clearly does.
pic.twitter.com/X7R7bT8FEi
Disease prevention ranges from vaccinations to early detection of cancer through screening. These are just examples and public health policies change as new threats to health emerge and more scientific knowledge is established.
When the NHS was set up in 1948, the intention was not just to treat ill-health but to prevent it. The founding White Paper put it like this: “Personal health still tends to be regarded as something to be treated when at fault… but seldom as something to be positively improved and promoted”.
Research (pre-pandemic) published in the British Medical Journal calculated that every extra £ spent on prevention was three to four times as effective as spending on curative services (in terms of “quality adjusted life years”).
Cuba is well known for its preventative approach to health care. It has the highest rate of doctors to population in the world – more than three times the United States. Each doctor and nurse team, embedded in the community, looks after about 300 families through a network of 15,000 clinics and over 400 polyclinics. Remarkably for a country with less than one eighth of the gross national income per person as the US, Cuba has had a lower rate of infant mortality for the last twenty years.
The Health Foundation calculated that a major part of the public health budget in England has been cut in real terms by 24% since 2015/6. This refers to the public health grant that English local authorities get to provide a range of preventive services around child health, obesity, drugs and alcohol, and smoking. The latter has been cut by 41% and drug and alcohol services by 28%. This matters for us because all categories of public health spending for England are matched at 100% for the North of Ireland under the Barnett formula.
The degrading of public health was exposed by the pandemic. Although seven pandemic “war games” had been run between 2015 and 2018 – including one for the MERS Coronavirus and another for H2N2 Influenza – the lessons weren’t implemented, especially regarding stocks of protective equipment and care home capacity. Jeremy Hunt, who was Health secretary for Exercise Cygnus, apparently walked out when confronted with a decision to switch off ventilators and redeploy health staff elsewhere. The government has fought hard to prevent public disclosure of the reports on these exercises.
Comparing life expectancy in UK and Ireland shows two things. That the UK has had a significant #publichealth crisis in the last 10 years and, also, just how badly the UK dealt with #COVID19 in its first year compared with our nearest neighbour pic.twitter.com/b3CN8iYPVE
— Dr Gabriel Scally (@GabrielScally) July 12, 2022
Recent British governments have been actively hostile to public health initiatives. For example, England has not introduced alcohol minimum unit pricing (MUP), whereas Scotland and Wales have. The Republic implemented MUP a year ago (€1 per unit), having delayed in the vain hope that the North would do the same and at a similar time. MUP is hardly a radical policy. Last week the Canadian Centre on Substance Use and Addiction recommended that people had no more than two drinks a week, and preferably gave up alcohol altogether because of the risks of cancer, strokes and heart disease.
Another example of hostility to public health measures concerns sugar. Taxing sugar in fizzy drinks is now common in many countries as an incentive for companies to lower sugar content. The aim is to reduce tooth decay and obesity in children. The Republic introduced a Sugar Sweetened Drinks Tax in 2018 at the same time as the application of the UK-wide Soft Drinks Industry Levy. In July 2021, a broader sugar tax of £3 per kilo was proposed as one of the recommendations in the UK’s National Food Strategy. The Strategy said that bad diets were causing 64,000 deaths a year. Johnson immediately dismissed the sugar tax idea, along with the proposed salt tax. And when Liz Truss took over she initiated a review of all policies designed to reduce consumption of sugar, salt and highly processed “junk” food, given her belief that the “nanny state” should not be restricting the freedoms of food and drink companies.
When you have a National Health Service, paid by all of us, there must be better public health yet Liz Truss scraps sugar tax. Even a marginal reduction in obesity would free a huge chunk of primary and secondary care. We drink too much, eat too much, exercise too little…… pic.twitter.com/sjpk8kWNUM
— David Yelland (@davidyelland) September 15, 2022
The Food Strategy also proposed several measures designed to address the climate emergency. It argued that, “our eating habits are destroying the environment”, mainly through the production and consumption of meat. It cautiously recommended cutting meat consumption by a third over the next ten years. But “after pressure from a small group of right wing backbenchers”… the strategy is being watered down.
New - the upcoming food strategy which was hoped to be ground breaking blueprint for tackling obesity, food poverty & nature & climate emergency is being watered down to empty sound bites according to those who fed into the white paper https://t.co/MYgeazydtd
— Helena Horton (@horton_official) June 7, 2022
The food chain is not the only health and environmental threat. Air pollution, both inside and outside of the home, is responsible for 7 million premature deaths a year globally, or 1,300 in Ireland (South) and probably another 500 in Ireland (North). The World Health Organization revised the standards in 2021, following a review that found strong evidence that, “air pollution may be damaging every organ in the body, causing heart and lung disease, diabetes and dementia and reducing intelligence”.
While Ireland meets the lower EU legal air quality standards – see here for daily monitoring (https://airquality.ie) – it does not meet the new health-based WHO guidelines for particulate matter and gases such as nitrogen dioxide (for the North put your postcode into this app which uses the latest WHO standards: addresspollution.org ). Vehicles and heating systems burning fossil fuels are the main cause of air pollution.
We urgently need to tackle engine idling in Ireland.
— IrishEVs (@IrishEVs) February 21, 2021
Travel to any small town and you'll regularly see multiple vehicles idling- often without anyone in them.
The emissions from engine idling is huge - and switching off saves money too!https://t.co/bV6Lz5wHuj pic.twitter.com/yczwjfGY5Z
Brexit bonus alert: Westminster’s attempted bonfire of EU law may well do away with the legal commitment to achieve the old EU standards. In any case, last month the British government extended the deadline for meeting those standards to 2040. No wonder there is a private member’s bill at Westminster to “establish the right to breathe clean air” – The Clean Air (Human Rights) Bill. Note that hostility to air quality standards is suspended when it comes to MPs’ self-interest – special air filtration has been installed at Westminster. And we haven’t got on to microplastic pollution yet.
So, after a vaccine only approach with advice mainly to wash hands & circulate air (open windows & get a foundering) we find a ventilation system has been installed in the House of Commons.
— Carol McCullough 🦓 ⚡🐬 (@Imonlyslightly) January 19, 2023
School children don't matter. Sure it's only the plebs.
This sounds about right. pic.twitter.com/q99ByUt9Wt
There is a statistic that sums up the state of both preventive and curative health care. It is the number of deaths per 100,000 population (aged under 75) that could be “mainly avoided” through public health and primary prevention measures (“preventable”), and through timely screening and health care (“treatable”). In 2018 the rate of total avoidable deaths in the North was 254 compared to 172 in the South (UK = 204). The preventable death rate was 172 in the North and 109 in the South (UK = 129). Sure, getting rid of the protocol will fix all that.